Since its launch in 2016, Crohn’s and Colitis Canada’s Promoting Access and Care through Centres of Excellence (PACE) program has connected Crohn’s and colitis specialists from across the country to share insights and improve the level of care available to people living with inflammatory bowel disease (IBD).
The PACE program integrates research and patient care in order to address healthcare gaps affecting Canadians living with Crohn’s disease or ulcerative colitis. The program focuses on four key areas of IBD care, and links five Canadian IBD Centres of Excellence: The University of Calgary, the University of Alberta, McMaster University, McGill University, and Mount Sinai Hospital.
Here’s a look at what PACE researchers achieved in the program’s second year, and what to expect in year three.
Servicing remote communities through telemedicine
Researchers at Toronto’s Mount Sinai Hospital are enabling people with IBD living in rural and remote areas to access consultations with healthcare specialists via video teleconferencing. In the past year, researchers increased the number of patients accessing telemedicine from 50 to 128, and increased the number of IBD
Ontario Telemedicine Network (OTN) locations from 33 to 55. The PACE telemedicine program has also enabled new IBD consultations to be scheduled within approximately 17 days of referral, and 83% of patients with active IBD symptoms are seen within 2 weeks.
“
I needed specialized care because of my complex disease. My family and I now have peace of mind because I have access to specialists who understand complex cases, without having to travel the long distance to the city.”
- Susan Foulds
PACE IBD Telemedicine Program participant
Nipigon, Ontario
Also in year two, patients participating in the telemedicine program started using the
HealthPROMISE application, which allows patients and healthcare professionals to monitor symptoms and quality of life scores between planned clinic visits.
In the coming year, the PACE IBD Telemedicine Program will expand to serve more patients, employ more OTN locations and increase the utilization of the HealthPROMISE program.
Monitoring patient health between visits
Patients increasingly want to be more involved in their care. At the same time, IBD specialists see the value in having more regular contact with patients to better monitor symptoms. To address both areas, researchers from McMaster University worked with Sinai AppLab to customize a mobile app called HealthPROMISE. The app allows patients to report their symptoms and quality of life markers between planned clinic visits. Users can also find educational resources within the app. Physicians and nurses will be able to receive patient-entered information electronically, track symptoms and medication adherence, and determine who may need additional care or referral to other specialists.
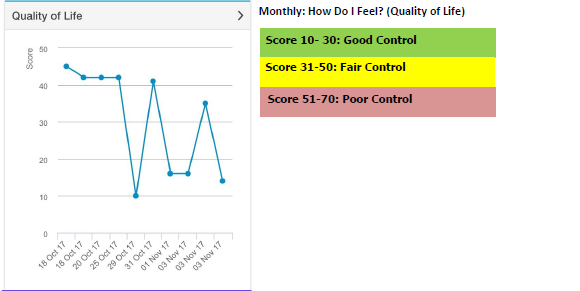 The HealthPROMISE app allows patients and their medical team to track quality of life scores over time.
The HealthPROMISE app allows patients and their medical team to track quality of life scores over time.
The HealthPROMISE app was launched as pilot projects at McMaster University, Mount Sinai Hospital, and the McGill University Health Centre. These pilot projects will carry on into year three of PACE, and continue recruiting users to determine whether the app improves quality of care and patient satisfaction.
Reducing chronic steroid use
The repeated use of steroids to treat Crohn’s or colitis can lead to serious complications. Researchers from the Universities of Calgary and Alberta are aiming to minimize the repeated use of steroids, and have developed care standards applicable to all Canadians living with IBD.
In their second year with PACE, these researchers implemented a series of Clinical Care Pathways (CCPs), which translate practice guidelines into user-friendly tools for clinicians. Researchers developed 16 checklists with input from IBD patients, specialists, and published data.
The CCPs were designed to help minimize exposure to systemic corticosteroids and reduce delays in starting patients on biologic treatments. Access to the CCPs will allow IBD care providers to deliver the same standard of care to all their patients, based on the most up-to-date clinical practice guidelines.
In year three of the PACE program, the team in Alberta will evaluate the impact of the CCPs on IBD flare management and corticosteroid administration.
Measuring healthcare advances
To improve the quality of care delivered to all Canadians with IBD, researchers from McGill University have developed a list of 45 quality indicators (QIs) that will act as benchmarks for an IBD clinic to measure how well it is delivering patient-centred care. Patients were consulted in the development of the QIs to ensure their specific concerns were addressed.
Researchers collaborated with the
Canadian Association of Gastroenterology (CAG) to develop the first IBD Global Rating Scale (GRS). The IBD GRS will help clinics and healthcare professionals assess the quality of service they provide by assigning letter grades from A to D to the quality of clinical care and patient experience. This initiative encourages IBD clinics to evaluate and assess their practice on an ongoing basis, and take steps to improve where necessary.
The next phase of this project is to pilot the QIs and IBD GRS to give researchers a better idea of what a wider roll out to hospitals and community clinics would look like. The PACE centres,
Canadian IBD Network for Research and Growth in Quality Improvement (CINERGI) group centres, and community hospitals will be recruited to pilot these quality initiatives.
Donations to Crohn’s and Colitis Canada allow the PACE network to carry on its vital work and elevate inflammatory bowel disease care. To find out more about how you can contribute to PACE, contact Katy Devitt, Manager of Research Programs at Crohn’s and Colitis Canada.